Female Genital Tuberculosis (FGTB) affects women’s reproductive health. Learn about its symptoms, diagnosis, and treatment for genital TB in India, and how it impacts fertility.
Female Genital tuberculosis (TB) is a significant health concern in India, especially among women of reproductive age. In developing countries like ours, the burden of tuberculosis remains high, making it crucial to understand the symptoms, causes, diagnosis, and treatment options for genital TB.
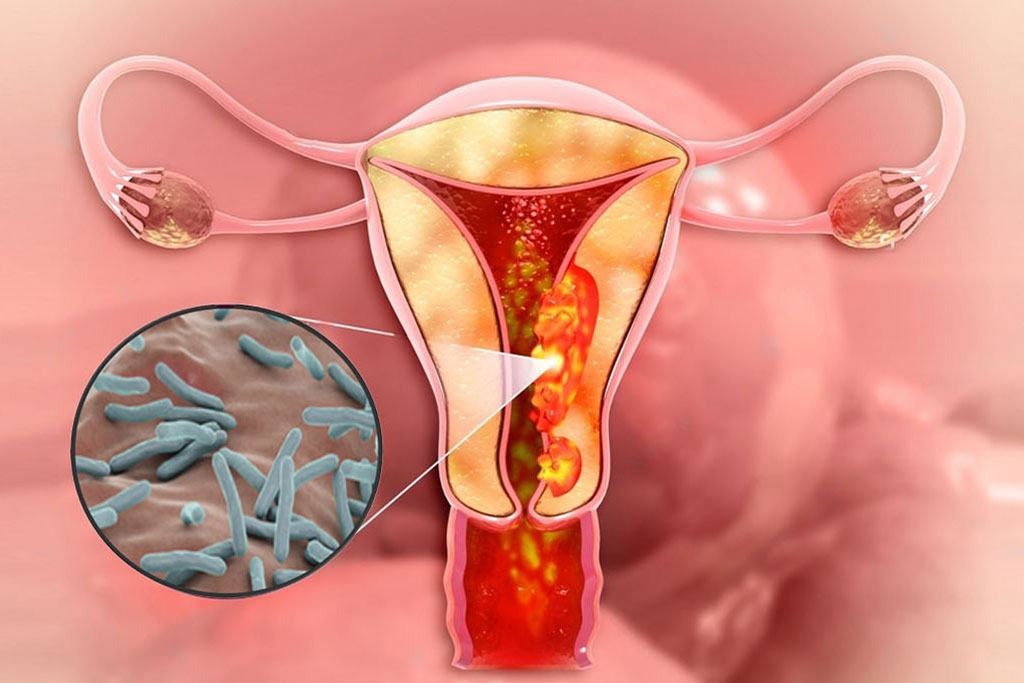
What is Genital Tuberculosis?
Genital tuberculosis is a form of extrapulmonary TB caused by the bacterium Mycobacterium tuberculosis. While TB primarily affects the lungs, it can spread through the bloodstream or lymphatic system to other organs, including the reproductive system. In females, genital TB typically targets the fallopian tubes, uterus, ovaries, and cervix, leading to serious complications such as infertility. Male genital TB, although less common, can affect the testes, prostate, and seminal vesicles.
How Does Genital TB Spread?
Genital tuberculosis usually originates from a primary TB infection in the lungs. The bacteria travel via the bloodstream or lymphatic system to the pelvic and genital areas. Key modes of transmission include:
- Hematogenous spread: TB bacteria travel through the blood.
- Lymphatic spread: Infection spreads through the lymph nodes.
- Sexual transmission: Though rare, sexual transmission can occur if a male partner has active genitourinary tuberculosis.
Causes of Genital Tuberculosis
The primary cause of genital tuberculosis is an untreated or inadequately treated pulmonary TB infection. In India, where TB prevalence is high, other contributing factors include:
- Low immunity: Conditions like malnutrition, HIV/AIDS, and diabetes weaken the immune system.
- Close contact with TB patients: Prolonged exposure to someone with active TB increases the risk.
- Poor living conditions: Overcrowding and poor ventilation facilitate the spread of TB.
Early Symptoms of Female Genital TB

Female genital tuberculosis symptoms can be subtle and often resemble other gynecological conditions, making early diagnosis challenging. Common symptoms include:
- Irregular or missed periods (amenorrhea)
- Lower abdominal or pelvic pain
- Abnormal vaginal discharge
- Pain during intercourse (dyspareunia)
- Infertility (primary or secondary)
- Systemic signs such as low-grade fever, fatigue, and unintended weight loss
Symptoms of Male Genital TB
- Pain in the groin or testicles
- Painful urination
- Inflammation or swelling of the testicles
- Blood in the urine or semen
Diagnosis of Genital Tuberculosis
Early detection of genital TB is essential to prevent complications. Diagnostic procedures include:
- Tuberculin Skin Test (Mantoux test): A small amount of TB protein is injected under the skin, and the reaction is observed after 48-72 hours. A positive result indicates TB exposure but does not confirm active disease.
- Hysteroscopy: A thin tube with a camera is inserted into the uterus to examine the uterine lining and detect abnormalities.
- Laparoscopy: This minimally invasive procedure allows doctors to inspect the pelvic organs and collect biopsy samples for analysis.
- PCR Test: Polymerase chain reaction (PCR) helps detect TB bacteria by amplifying their genetic material.
- Ultrasound Scans: Used to examine the pelvic region for abnormalities.
- Endometrial Biopsy: A sample of the uterine lining is taken and tested for TB.
Complications of Genital TB
Untreated or poorly managed genital TB can lead to:
- Scarring and blockage of fallopian tubes
- Uterine deformities
- Chronic pelvic pain
- Ectopic pregnancies
- Permanent infertility

Treatment & Management of Genital TB
The treatment protocol for genital tuberculosis is similar to that of pulmonary TB. It involves a combination of anti-TB medications for a duration of 6 to 12 months. The standard regimen includes:
- Isoniazid (INH)
- Rifampicin (RIF)
- Pyrazinamide (PZA)
- Ethambutol (EMB)
Patients must complete the full course of treatment to prevent drug resistance and ensure complete recovery.
Can I Conceive After Genital TB Treatment?
Yes, conception is possible after successful treatment of genital TB. However, it depends on the extent of damage to the reproductive organs. Women with mild to moderate damage may conceive naturally or with the help of assisted reproductive techniques like IVF. In severe cases, where the fallopian tubes are irreparably damaged, IVF using frozen embryos might be the only option.
Genital Tuberculosis and Infertility
Genital tuberculosis is a leading cause of infertility in Indian women. The infection damages the fallopian tubes, ovaries, and uterine lining, reducing the chances of natural conception. Regular screenings, early diagnosis, and prompt treatment can help prevent infertility caused by TB.
Preventing Genital TB
Prevention is always better than cure. Here are some tips to prevent genital TB:
- Get vaccinated: The BCG vaccine, administered at birth, offers partial protection against TB.
- Strengthen your immune system: A balanced diet rich in fruits, vegetables, and proteins helps boost immunity.
- Avoid close contact with TB patients: If unavoidable, wear a mask and ensure proper ventilation.
- Practice safe sex: Use condoms to reduce the risk of sexually transmitted infections, including TB.
- Regular medical check-ups: If you have a family history of TB or experience any symptoms, consult a doctor promptly.
Female genital tuberculosis is a serious condition that can have long-term consequences, including infertility. However, with early diagnosis and proper treatment, many women can recover fully and even conceive. In India, raising awareness about genital TB and improving access to healthcare services are key to reducing its prevalence. If you suspect any symptoms, don’t hesitate to seek medical advice.
For more health-related content, stay tuned to our blog. Written by Samruddhi Sathe, this article aims to empower readers with the knowledge needed to tackle health issues effectively.
References:
- Sharma J.B. et al.; “Current Diagnosis and Management of Female Genital Tuberculosis,” PubMed Central.
- Grace G.A., Devaleenal D.B.; “Genital Tuberculosis in Females,” Indian Journal of Medical Research.
- Yadav S. et al.; “Genital Tuberculosis: Diagnosis and Management,” AIIMS.
Also Read:
Role of Zygote in Fetal Development
5 Best Yoga Poses for Pregnancy: Instant Relaxation at Work
Comprehensive Guide to Understanding Health Insurance



Pingback: Polycystic Ovarian Syndrome (PCOS) in India – Symptoms, Causes, & Pregnancy Guide